 Holistic nursing care is a concept that moves away from viewing a patient as merely a 'diagnosis'; rather, the patient is viewed and treated as a whole person. In other words, holistic nursing will involve care and support of the person's physical, mental, spiritual, emotional, social and environmental needs. In many cases, holistic nursing may also include alternative therapies that may be seen as beneficial, with the patient's consent. This is not a new concept—even Florence Nightingale advocated holistic nursing: "Florence Nightingale recognized the importance of caring for the whole person and encouraged interventions that enhanced individuals' abilities to draw upon their own healing powers. She considered touch, light, aromatics, empathetic listening, music, quiet reflection, and similar healing measures as essential ingredients to good nursing care." - American Holistic Nurses Association (AHNA), Position Statements, 2004 One of the most important aspects of holistic care is the involvement of the patient in making their own decisions, always being allowed to consent or deny a route of care, and a focus on self-care where ever possible. Holistic nursing not only involves those patients with curable illness but for terminal illness as well. Take any factor within holistic care—physical, psychological and emotional, spiritual and environmental aspects of life—each individual aspect has an effect on the mental and physical health of a patient. They are all interconnected and related to the person as whole. Where one area is not understood or assisted then true healing or care can't take place.A holistic assessment is one that not only identifies the care required for health requirements but the impact that other areas of the patient's life may be impacting on the path of treatment and/or cure. Holistic nursing assessments are an excellent way to identify the true needs of a patient because they:
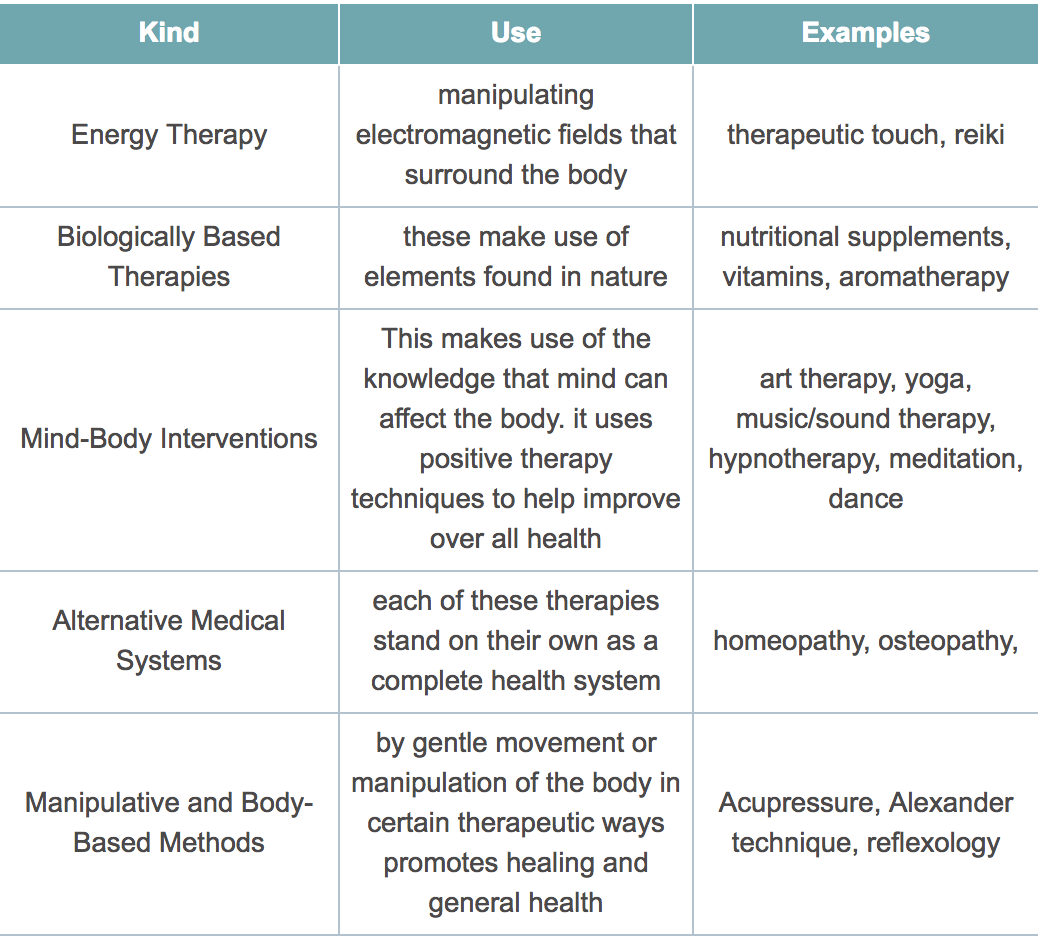
Holistic Nursing Care and Alternative Therapies Nurses who have received the proper training often incorporate alternative therapies into treatments along with conventional medicine. There are a huge variety of alternative treatments available today - not all suitable for all patients. Therefore during the holistic nursing assessment it may become clear what alternative therapies might be available if the patient is in agreement about trying them. The table below highlights some of the main therapies and the broad reasons why they are used. So what exactly is Holistic Nursing Care?
I hope that this short article has given you a better idea of what holistic care should be about. More importantly I hope that you have realised that, if you ever need health care, you do have a right to make choices, make decisions and be involved every step of the way when it's your health and your life that's involved. Nurses and patients shouldn't be on different sides of the fence. It should be a partnership. A partnership based on mutual trust, respect and honesty. It has been many years since I stepped foot onto my first surgical ward during my nurse training. The first words I heard were spoken by a trained nurse in front of the patient and his family, speaking to another nurse, she nodded towards the patient and said "Could you admit this 'appendectomy' now". I couldn't help but think at that moment how I would feel if I was addressed as a mere condition to be admitted, sorted and then thrown out. Thankfully, with an holistic nursing care approach this kind of off-hand thinking has no place. author - Helen Murphy Howell
2 Comments
 The first step to finding the best senior housing for your loved one is to understand what type of care facility is the best fit. There are six main types of residential elder care options: Independent living facilities are ofen the best senior housing options for active adults who want built-in community without giving up their privacy. Most feature studio or multi-bedroom apartments with kitchens so residents can stay independent as long as possible. Continuing care retirement communities, or CCRCs, are best for those seeking a continuum of care from independent living to skilled nursing, all in one location. CCRCs generally have studio or multi-bedroom apartments for their most independent residents and private or shared rooms for residents who need more care. Assisted living facilities are best for for those who need some care and supervision but who don't need skilled nursing care. Most assisted living residents live in private or semi-private rooms within a complex. Memory care communities are facilities designed specifically for seniors with Alzheimer’s disease or other forms of dementia or serious cognitive impairments. Also known as dementia care, memory care communities are often housed in one part of an existing assisted living community or skilled nursing facility. These communities are best for those with severe dementia or cognitive impairment who are no longer able to live independently. Board and care facilities, also known as care homes, are best for those who can't live independently due to physical or mental disabilities but who don't require fulltime skilled nursing care. They feature private or semi-private rooms in a complex (often a large home) that usually provides communal dining. Skilled nursing facilities, also called nursing homes, are residential care facilities that are best for those with illnesses or mental conditions requiring fulltime monitoring and medical care. Most skilled nursing residents live in semi-private rooms, and meals are generally provided. If your are confused, give us a call! We're more than happy to help. The decision to help an aging adult move out of a current home is a complex one -- both emotionally and practically. Above all, you want the person to be safe and well. How can you all feel more confident about whether circumstances suggest that your loved one should no longer be living alone?
Although every situation is different, looking at the following 11 signs will give you valuable information to help make the decision. 1. Big-picture signs it might be time for assisted livingKeep the big red flags in mind. Certain situations make it more obvious that it's wise to start thinking about alternate living arrangements. Look for:
Look for:
Look for:
Look for:
Look for:
Look for:
Look for:
Look for:
Look for:
Look for:
Look for:
If, on the other hand, your loved one is showing signs that living alone is a strain, it may be time for a talk. Broach the subject of where to live in a neutral way and you may find that your loved one harbors the same fears for current and future safety and security that you do. Find out what your loved one fears most about moving and about staying before launching into your own worries and what you think ought to be done. Dementias are degenerative disorders that develop primarily in the nervous system and selectively damage particular areas of the brain. Some dementias, like Alzheimer’s disease affect all areas of the brain simultaneously, while others, such as frontotemporal dementia, affect the parts of the brain involved in controlling one’s communications and emotions. Still others are caused by vascular disease, brain trauma, or chronic alcohol abuse (Korsakoff’s syndrome)
By 2030, 20% of U.S. population will be older than 65 years of age – about 50 million people. Dementia affects 1% to 6% of those older than 65, and between 10% and 20% of those older than 80 years of age. In the next 30 years, estimated 10-20 million seniors in U.S. will have mild to severe forms of dementia. Seniors with history of moderate traumatic brain injury (TBI) have a 2-3 times greater risk of developing Alzheimer’s disease – those with a severe TBI have a 4-5 times greater risk. Even healthy seniors are at risk for falls and head trauma, so any fall to the head, however minor, should be seen by a medical professional and documented. Alzheimer’s disease accounts for 65% of all dementias. There is no direct diagnosis of Alzheimer’s – and while PET scans and other imaging techniques are being studied, none have yet been able to show the presence of Alzheimer’s disease. Alzheimer’s onset often surprises families because vision, movement, and sensation remain untouched while a senior’s memories begin to slowly decrease. Recent memories are affected first, leading to “senior moments” that appear innocent because all other memories, including those from decades ago, remain intact. Eventually those remote memories begin to fade, and lastly the senior’s “crystallized” memories, such as family member’s names and faces, are compromised. By David L. Raffle, PhD Clinical and Forensic Neuropsychologist www.RaffleBrainInstitute.com When a loved one reaches a point in his or her life in which self-care becomes challenging, the next step may be a little overwhelming; particularly when trying to make the best choice for your loved one and your family. Some families struggle with guilt because it may not be financially, emotionally, or physically feasible for some individuals to become a caregiver. Often times a hired in-home caregiver is only a temporary solution until the aging or ill loved one requires more specialized care. Unfortunately, more often than not, many people are hesitant to choose the most common option of a nursing home facility due to the horror stories or bad reputations they can have.
Although a nursing home can be an intimidating next step, if you know what to look for and monitor closely, your elderly loved one can continue to live a healthy and safe life. Myth #1: Nursing Homes Mark the “Final Days” of an Elderly Individual While it is true that many elderly individuals may live their final years in a nursing home, it doesn’t automatically mean that an elder is living his or her last days. A nursing home is not a hospital, as it often mistaken for, but does have medically trained staff available 24 hours a day. Nursing home candidates do not need to be in a hospital, but are no longer to be cared for in their home or cannot take care of themselves. Although a majority of nursing home residents are older seniors, some younger seniors have short stays in a nursing home after a lengthy illness or after a surgery. Myth #2: “If I move my elderly relative into a nursing home, he’ll lose all of his independence.” When selecting a nursing home, many are fearful to move someone into a facility out of fear that he or she will have no independence. Many facilities respect and even encourage independence as much as possible. Even if one individual may have mobility issues, the staff will encourage other independent activities such as eating, grooming, and participating in activities. When deciding on whether or not to move your loved one into the appropriate care, keep in mind that the need for assistance is not the result of a loss of independence as we all require help sometimes. Myth #3: “If my loved one moves into a nursing home, she will be mistreated by staff and there will be nothing I can do.” We’ve all heard the terrible stories of nursing home abuse or elder abuse. Unfortunately, these stories of physical, emotional, and financial mistreatment are true, but they don’t apply to every nursing home facility across the country. First off, the best way to prevent elder abuse from occurring is by being active in your elder’s life. Before you choose a facility, take a tour, look around, and ask questions because this is the time in which you are interviewing facilities in search of the best possible care your loved one can receive. If anything feels or looks wrong, you don’t have to settle for that particular home. Be sure to educate yourself on how to recognize and respond to any sign mistreatment of your loved one. Once you have found a suitable home for your elder, visit often, communicate regularly with staff, keep track of any changes to physical appearance and his or her emotional or mental state. Changes could be part of aging, but it could also indicate abuse. If you suspect any abuse, contact authorities immediately. This next chapter in your loved one’s life can be a positive transition and an opportunity to feel confident that they are being provided with the best care and surrounded by friends and family. |
ArticlesRead important articles and blogs from respected authorities and first-hand experience. Archives
July 2018
Categories |


 RSS Feed
RSS Feed
